Abstract
Literature Review
Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting Children
Erwin Gunawan* and Ria Puspitawati
Published: 24 December, 2024 | Volume 8 - Issue 1 | Pages: 059-065
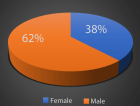
Background: Stunting is a condition of growth and development disorders in children under 5 years of age who appear shorter than their age caused by nutritional deficiencies. The stunted growth and development of children can be influenced by deficiencies in the intake of macronutrients such as protein and micronutrients such as calcium, phosphorus, zinc, and vitamin D. One nutrient that is relevant to current dental health research is vitamin D.
Objective: This review article will further analyze the relationship between vitamin D deficiency and Porphyromonas gingivalis bacterial lipopolysaccharide in stunting children.
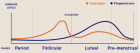
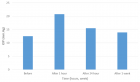
Literature review: Vitamin D deficiency can cause various problems related to the oral cavity such as a decrease in salivary flow rate, buffer capacity, and salivary content such as protein. A decrease in salivary flow rate causes secretory Immunoglobulin A (IgA) to decrease, thus disrupting the colonization of normal microflora in the oral cavity. Reduced vitamin D levels can potentially increase the number of Porpyhromonas gingivalis bacteria and also lipopolysaccharides (LPS), thus inhibiting the proliferation and differentiation of alveolar bone cells.
Conclusion: Therefore, lack of micronutrient intake such as vitamin D deficiency can trigger the growth of Porphyromonas gingivalis bacteria and an increase in bacterial products such as lipopolysaccharides, especially in stunted children.
Read Full Article HTML DOI: 10.29328/journal.abse.1001033 Cite this Article Read Full Article PDF
Keywords:
Lipopolysaccharide; Porpyhromonas gingivalis; Stunting; Vitamin D
References
- Kesuma ZM, Siregar LR, Fradinata E, Fathimah A. Factors affecting stunting in children under 5 years of age in Indonesia using spatial model. Indian J Public Health. 2022;66(3):264. Available from: https://doi.org/10.4103/ijph.ijph_1989_21
- Minervini G, Franco R, Marrapodi MM, Blasio MD, Ronsivalle V, Cicciu M. Children oral health and parents education status: a cross-sectional study. BMC Oral Health. 2023;23(787):2-7. Available from: https://doi.org/10.1186/s12903-023-03424-x
- Reis CLB, Barbosa MCF, Henklein S, Madalena IR, Lima DC, Oliveira MA, et al. Nutritional status is associated with permanent tooth eruption in a group of Brazilian school children. Glob Pediatr Health. 2021;8:1-6. Available from: https://doi.org/10.1177/2333794X211034088
- Kustanto A. The prevalence of stunting, poverty, and economic growth in Indonesia: a dynamic panel data causality analysis. J Develop Econ. 2021;6(2):150173. Available from: https://doi.org/10.20473/jde.v6i2.22358
- Heo JS, Ahn YM, Kim AE, Shin SM. Breastfeeding and vitamin D. Clin Exp Pediatr. 2022;65:418–29. Available from: https://doi.org/10.3345/cep.2021.00444
- Trave TD, Victoriano FG. Pregnancy, breastfeeding, and vitamin D. Int J Mol Sci. 2023;24(11881):2. Available from: https://doi.org/10.3390/ijms241511881
- Cicek H, Duyuran R, Sri RMM, Ravichandran S. Biochemistry and metabolism of vitamin D. Int J Clin Biochem Res. 2023;10(1):28-36. Available from: https://doi.org/10.18231/j.ijcbr.2023.005
- Alhelfi NM, Hoobi NM. Effect of vitamin D deficiency on dental caries and salivary parameters. J Med Chem Sci. 2023;6(6):1363. Available from: https://doi.org/10.26655/JMCHEMSCI.2023.6.16
- Babina K, Salikhova D, Polyakova M, Svitich O, Samoylikov R, El-Abed SA, et al. The effect of oral probiotics (Streptococcus salivarius K12) on the salivary level of secretory immunoglobulin A, salivation rate, and oral biofilm: a pilot randomized clinical trial. Nutrients. 2022;14(1124):1-13. Available from: https://doi.org/10.3390/nu14051124
- Almahmoud E, Alkazemi DUZ, Al-Qabandi W. Growth stunting and nutritional deficiencies among children and adolescents with celiac disease in Kuwait: a case-control study. Children. 2024;11(1042):1-17. Available from: https://doi.org/10.3390/children11091042
- Suryani D, Kusdalinah, Pratiwi BA, Yandrizal. Differences in macronutrient and micronutrient intake of stunted toddlers in rural and urban areas of Bengkulu Province. Nat Nutr J. 2024;19(ISP):68-75. Available from: https://orcid.org/0000-0003-0056-8328
- Martias I, Daswito R, Mukodri DML. Does water, hygiene, and sanitation indeed directly affect children’s stunting?: a scoping review. Int J Soc Sci. 2024;4(4):341-354. Available from: https://doi.org/10.53625/ijss.v4i4.8894
- Nazri NS, Vanoh D, Leng SK. Malnutrition, low diet quality and its risk factors among older adults with low socioeconomic status: a scoping review. Nutr Res Rev. 2021;34:107. Available from: https://doi.org/10.1017/s0954422420000189
- Chen S, Richardson S, Kong Y, Ma N, Zhao A, Song Y, et al. Association between parental education and simultaneous malnutrition among parents and children in 45 low-and middle-income countries. JAMA Netw Open. 2023;6(1):2. Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2800722#google_vignette
- Theodorea CF, Diven S, Hendrawan D, Djais AA, Bachtiar BM, Widyarman AS, Seneviratne CJ. Characterization of oral Veillonella species in dental biofilms in healthy and stunted groups of children aged 6–7 years in East Nusa Tenggara. Int J Environ Res Public Health. 2022;19(13998):1-9. Available from: https://doi.org/10.3390/ijerph192113998
- Hernández P, Sánchez MC, Llama-Palacios A, Ciudad MJ, Collado L. Strategies to combat caries by maintaining the integrity of biofilm and homeostasis during the rapid phase of supragingival plaque formation. Antibiotics. 2022;11:880. Available from: https://doi.org/10.3390/antibiotics11070880
- Thomas C, Minty M, Vinel A, Canceill T, Loubières P, Burcelin R, et al. Oral microbiota: A major player in the diagnosis of systemic diseases. Diagnostics. 2021;11:1376. Available from: https://doi.org/10.3390/diagnostics11081376
- Deo PN, Deshmukh RS. Oral microbiome research – a beginner’s glossary. J Oral Maxillofac Pathol. 2022;26(1):87. Available from: https://doi.org/10.4103/jomfp.jomfp_455_21
- Wang J, Feng J, Zhu Y, Li D, Wang J, Chi W. Diversity and biogeography of human oral saliva microbial communities revealed by the Earth Microbiome Project. Front Microbiol. 2022;13. Available from: https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.931065/full
- Rajasekaran JJ, Krishnamurthy HK, Bosco J, Jayaraman V, Krishna K, Wang T, et al. Oral microbiome: A review of its impact on oral and systemic health. Microorganisms. 2024;12(1797):5-7. Available from: https://doi.org/10.3390/microorganisms12091797
- Arweiler NB, Rahmel V, Alashkar Alhamwe B, Alhamdan F, Zemlin M, Boutin S, et al. Dental biofilm and saliva microbiome and its interplay with pediatric allergies. Microorganisms. 2021;9(6). Available from: https://doi.org/10.3390/microorganisms9061330
- D’Agostino S, Ferrara E, Valentini G, Stoica SA, Dolci M. Exploring oral microbiome in healthy infants and children: A systematic review. Int J Environ Res Public Health. 2022;19:11403. Available from: https://doi.org/10.3390/ijerph191811403
- Aleksijevic LH, Aleksijevic M, Skrlec I, Sram M, Sram M, Talapko J. Porphyromonas gingivalis virulence factors and clinical significance in periodontal disease and coronary artery diseases. Pathogens. 2022;11(1173):1-19. Available from: https://doi.org/10.3390/pathogens11101173
- Kugaji M, Muddapur U, Bhat K, Joshi V, Manubolu M, Pathakoti K, Peram MR, Kumbar V. Variation in the occurrence of fimA genotypes of Porphyromonas gingivalis in periodontal health and disease. Int J Environ Res Public Health. 2020;17:1-2. Available from: https://www.mdpi.com/1660-4601/17/6/1826
- Zhang Z, Liu D, Liu S, Zhang S, Pan Y. The role of Porphyromonas gingivalis outer membrane vesicles in periodontal disease and related systemic diseases. Front Cell Infect Microbiol. 2021;10(585917):1-12. Available from: https://doi.org/10.3389/fcimb.2020.585917
- Fakhira FS, Garna H, Hadiati DE. Pengaruh defisiensi vitamin D terhadap proses pertumbuhan tulang pada balita stunting. Med Sci. 2023;3(1):860-62. Available from: https://doi.org/10.29313/bcsms.v3i1.6751
- Rosli NFH, Nor NSM, Adnan RA, Kadir SHSA. A review of vitamin D deficiency and vitamin D receptor polymorphisms in endocrine-related disorders. Clin Exp Pediatr. 2024;1-91. Available from: https://doi.org/10.3345/cep.2024.00227
- Picolo M, Stephen A, Baysan A. The antimicrobial effect of different vitamin D compounds on Streptococcus mutans and their impact on glycosyltransferase expression. J Oral Microbiol. 2024;16:1-12. Available from: https://doi.org/10.1080/20002297.2024.2327758
- Ji L, Gao J, Kong R, Gao Y, Ji X, Zhao D. Autophagy exerts pivotal roles in regulatory effects of 1α,25-(OH)₂D₃ on osteoclastogenesis. Biochem Biophys Res Commun. 2019;511:869-74. Available from: https://doi.org/10.1016/j.bbrc.2019.02.114
- Cao W, Li J, Yang K, Cao D. An overview of autophagy: mechanism, regulation, and research progress. Bull Cancer. 2021;108:304-322. Available from: https://doi.org/10.1016/j.bulcan.2020.11.004
- Dubey P, Mittal N. Periodontal diseases-a brief review. Int J Oral Health Dent. 2020;6(3):177-87. Available from: https://doi.org/10.18231/j.ijohd.2020.038
- Meza-Meza MR, Ruiz-Ballesteros AI, de la Cruz-Mosso U. Functional effects of vitamin D: From nutrient to immunomodulator. Crit Rev Food Sci Nutr. 2022;62(11):3042-3062. Available from: https://doi.org/10.1080/10408398.2020.1862753
- Salsabila N, Kasuma N, Yerizel E. Determinasi jumlah bakteri Porphyromonas gingivalis ATCC 33277 pada saliva anak stunting. e-GiGi. 2024;12(1):27. Available from: http://dx.doi.org/10.35790/eg.v12i1.47864
- Marchetti E, Pizzolante T, Americo LM, Bizzaro S, Quinzi V, Mummolo S. Periodontology Part 4: Periodontal disease in children and adolescents. Eur J Paediatr Dent. 2022;23(4):332. Available from: http://dx.doi.org/10.23804/ejpd.2022.23.04.14
- Lu EMC. The role of vitamin D in periodontal health and disease. J Periodontol Res. 2023;58:213-24. Available from: https://doi.org/10.1111/jre.13083
- Meghil MM, Cutler CW. Influence of vitamin D on periodontal inflammation: a review. Pathogens. 2023;12(1180):6-8. Available from: https://doi.org/10.3390/pathogens12091180
- Yang X, Niu L, Pan Y, Feng X, Liu J, Guo Y, Pan C, Geng F, Tang X. LL-37-induced autophagy contributed to the elimination of live Porphyromonas gingivalis internalized in keratinocytes. Front Cell Infect Microbiol. 2020;10:561761. Available from: https://doi.org/10.3389/fcimb.2020.561761
Figures:
Similar Articles
-
Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting ChildrenErwin Gunawan*,Ria Puspitawati. Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting Children. . 2024 doi: 10.29328/journal.abse.1001033; 8: 059-065
Recently Viewed
-
Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical TrialAnders Wänman*, Susanna Marklund, Negin Yekkalam. Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical Trial. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001046; 9: 001-008
-
Hygiene and Care Protocols for Implant-supported Dental Prostheses in Patients with DiabetesHakob Khachatryan, Emma Boshnaghyan, Sevak Papoyan, Gagik Hakobyan*. Hygiene and Care Protocols for Implant-supported Dental Prostheses in Patients with Diabetes. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001047; 9: 009-014
-
Advancing Oral Health and Craniofacial Science through Microchip ImplantsShekufeh Shafeie*. Advancing Oral Health and Craniofacial Science through Microchip Implants. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001048; 9: 015-018
-
Texture Analysis of Hard Tissue Changes after Sinus Lift Surgery with Allograft and XenograftMohammad Azimzadeh, Farzad Esmaeili, Narges Bayat, Kasra Rahimipour, Amir Ebrahimpour Tolouei*. Texture Analysis of Hard Tissue Changes after Sinus Lift Surgery with Allograft and Xenograft. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001049; 9: 019-022
-
Awareness and Knowledge of Specialists/Trainers and General Dental Practitioners about Medical-Related Osteonecrosis of the JawsAbdulhamit Taha Koca,Mustafa Bayhan,Yunus Ayberk Demir,Ayse Zeynep Zengin*. Awareness and Knowledge of Specialists/Trainers and General Dental Practitioners about Medical-Related Osteonecrosis of the Jaws. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001050; 9: 023-031
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."